Sweden is being touted as an example of a successful fight against COVID-19 without imposing strict social isolation measures. While it is true that Sweden was one of the few countries that did not impose severe lockdown protocols and procedures, how did Sweden fare regarding various COVID-19 outcomes?
First of all, it is not true that Sweden took a totally relaxed approach to COVID-19 by keeping all establishments open throughout the pandemic. Swedes were indeed less rigid in their approach at the beginning of the pandemic. However, after a series of local outbreaks, mask-wearing was made more compulsory during the later stages of the pandemic.
Sweden’s initial approach was in stark contrast to other countries in Europe and its Nordic neighbors such as Finland and Norway. Sweden relied on a system of voluntary compliance by the population. Most of the facilities, such as restaurants, public spaces, and schools, remained open in the beginning. It was alleged that Sweden thought at the beginning of the pandemic that COVID-19 would not affect the country just as the earlier SARS (severe acute respiratory syndrome) pandemic in 2003 had not. SARS progressed from Asia to the Americas but spared most European countries despite grave predictions. In contrast, COVID-19 spread like wildfire in Northern Italy at the end of February 2020. Despite these reports, Sweden relied on an approach focused on herd immunity. Swedes believed that lax controls would result in higher infection rates in the general population and consequent herd immunity. In reality, the results were disappointing: by October 2020, only 5 to 10 percent of the population showed antibody levels that could be translated to immunity to COVID-19.
Various institutions in Sweden were generally open in the beginning, yet the public was advised to work from home if possible and to limit travel. Social distancing was recommended but not enforced. People over 70 were advised to self-isolate. These recommendations were mostly voluntary and not strictly imposed like in other countries.
It is also a misnomer to characterize that all schools were kept open in Sweden during the entire pandemic. All primary schools (years 1–9) remained open throughout the pandemic. However, upper secondary schools (years 10–12, called gymnasium or high school) and universities were closed until the end of the summer of 2020. The initial laid-back approach gave way to stricter controls when COVID-19 outbreaks occurred in December 2020 and early 2021, despite the initiation of vaccinations. Restrictions were progressively tightened at this time. In early December 2020, high schools were also closed until early January.
During the first and second waves of COVID-19, Sweden had a higher number of deaths per million population compared to most of its neighboring countries. Even though Sweden fared better than most European countries during the third wave, the cumulative incidence of deaths due to COVID-19 per million population in Sweden remained high and was rather close to the U.S., which leads the mortality statistics, as seen in the following graph. In contrast, the cumulative mortality in Norway, another Nordic country with which Sweden shares population characteristics and health care systems, was much lower as seen in the graph.
There was some controversy about the lowest “excess deaths” recorded in Sweden during 2020–2022, indicating a lower excess mortality due to COVID-19. This is controversial, and the estimation of the excess deaths compared to the prior years is a very indirect measure of actual COVID-19 mortality and can be affected by various confounding factors. Because of the variable approach adopted by different countries to document COVID-19 deaths, especially at the beginning of the pandemic with a lack of proper testing, excess deaths during the pandemic period are an inexact measure of actual COVID-19 deaths.
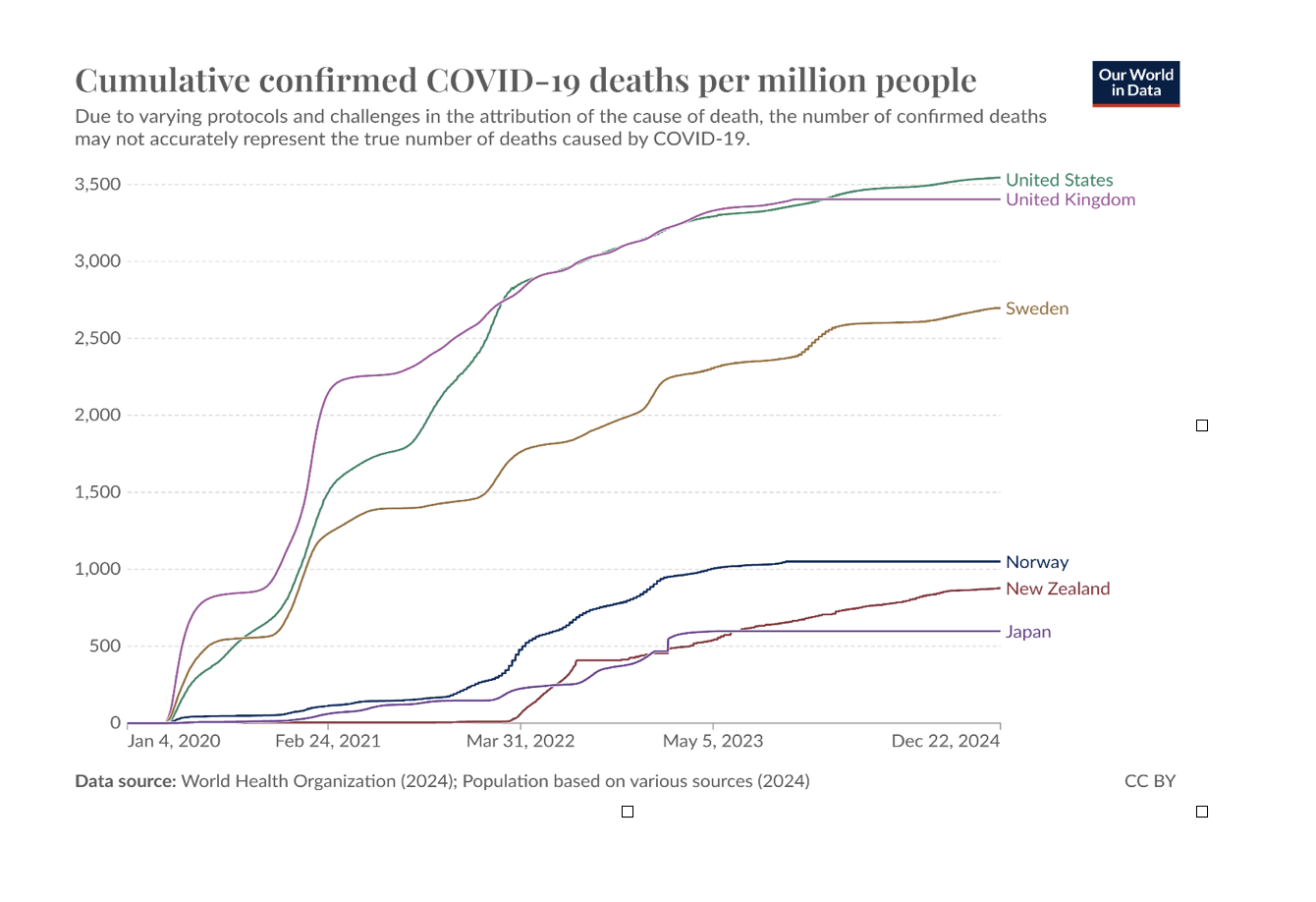
Total COVID-19 deaths per million population (2020–2024)
One of the troublesome consequences of Sweden’s approach was that 40 percent of all COVID-19 cases were recorded in older individuals aged more than 70 years. Most of the deceased lived in long-term care facilities. COVID-19 death rates were also higher among the poorer population.
A national COVID-19 commission was established early in the pandemic by the Swedish government to examine how Sweden handled the pandemic. They submitted their final report in 2022. According to the commission, the larger number of deaths in the older population was probably due to increased community transmission facilitated by the lack of rigorous community isolation protocols early in the pandemic. Interestingly, a national ban on visitors to long-term care facilities remained effective from April to October 2020, ostensibly to protect the most vulnerable individuals. This measure was found to have no effect on the transmission of COVID-19 in such facilities, probably because of the lax enforcement and the ability of staff to intermingle with the general population freely. In addition to the laid-back policies, other factors, such as a fragmented and decentralized infection control system, lack of testing supplies, and a higher proportion of the vulnerable population because of milder influenza during the preceding years, were also blamed for the higher number of COVID-19 deaths in elderly individuals. Although the committee faulted the government for slowness of response, they also concluded that not introducing lockdowns was fundamentally correct since it preserved “individual freedom.”
In a December 2020 interview, the king of Sweden, Carl XVI Gustaf, said, “I think we have failed. A large number have died, and that is terrible.” These facts do not agree with the narrative that Sweden’s “lax COVID-19 approach” resulted in reduced COVID-19 mortality. However, there is evidence that the adverse effects on early childhood education and development were not seen in Swedish children because most of the schools were kept open.
There are several caveats to consider before applying Swedish data to the U.S. Foremost, the population density of Sweden is only 26/km², whereas the U.S. has a population density of 38/km². The total Swedish population is only 10.5 million compared to 333 million in the U.S. Lower incidence of comorbidities such as diabetes and obesity should have caused a lower number of deaths in Sweden. Given these realities, Sweden should have fared much better compared to the U.S. The higher mortality proves that the relaxed approach of Sweden to COVID-19 was not a success.
Not implementing a mandatory lockdown was blamed for the higher mortality seen in Sweden. In a modeling study where researchers constructed an alternative version called “synthetic Sweden,” Cho found that the infection rates could have been reduced by 75 percent and mortality could have been reduced by 25 percent had Sweden imposed a strict lockdown during the initial phase of the pandemic.
P. Dileep Kumar is a board-certified practicing hospitalist specializing in internal medicine. Dr. Kumar is actively engaged with professional associations such as the American College of Physicians, Michigan State Medical Society, and the American Medical Association. He has held a variety of leadership roles and has authored more than 100 publications in various medical journals and a book on rabies (Biography of Disease Series). Additionally, he has presented more than 50 papers at various national and international medical conferences. Several of his papers are widely cited in the literature and referenced in various textbooks.